
This is the sixth post in our blog series taking a closer look at Connecticut’s behavioral health workforce challenges and their impact on children and families – and sharing solutions. Read the rest of the series here.
June 25, 2024
By Katie Newkirk, Ph.D., Senior Associate and Kellie Randall, Ph.D., Associate Vice President of Quality Improvement
If you work in the behavioral health field or have been following CHDI’s blog series this year, you know that Connecticut, like much of the country, is grappling with a post-pandemic surge in youth seeking mental health services coinciding with a serious shortage in the clinical workforce. Many of these young people will receive treatment at one of the state’s 22 outpatient psychiatric clinics for children (OPCCs), which CHDI has partnered with since 2009 to expand access to key evidence-based practices.
As our colleague Aleece Kelly recently explained, OPCCs are often the first stop, last stop, and holding zone for children and youth moving along the continuum of behavioral health services, playing a critical role in the system. But as Jack Lu described in an earlier post in this series, Connecticut’s OPCCs have been losing their most experienced clinicians at an alarming rate. As a result, more clinics are filling vacancies with less experienced staff.
While Dr. Lu’s post focused on strategies Connecticut can use to retain experienced staff, today we’ll explore the impact of this recent shift on this newer workforce and share strategies to support them as they navigate their new careers during this challenging time.
By providing more support for both experienced clinicians and those new to the field, we can ensure access to - and maintain the quality of – critical outpatient behavioral health services for children, youth and families.
As illustrated in Figure 1, the average number of youth served by Connecticut’s OPCCs has increased 20% in the last two years. Each provider served an average of 1,250 youth in fiscal year 2023, compared to 2019’s average of 1,034. 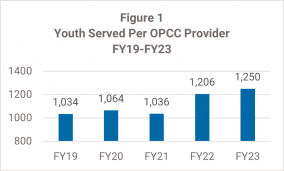
Even before the pandemic, adjusting to this growing demand would have been challenging. But new clinicians who trained during the pandemic are entering the field with less face-to-face experience than their earlier counterparts, due to necessary shifts to remote field placements and, for many, substituting simulations for field hours.
“Prior to COVID, we had a steady group of clinicians who had been with us for a long time. But after COVID, a lot of our more seasoned clinicians [went] into private practice,” says Melissa Jacob, LCSW, Director of Child Outpatient Services and Care Coordination at Bridges Healthcare, a Milford-based OPCC.
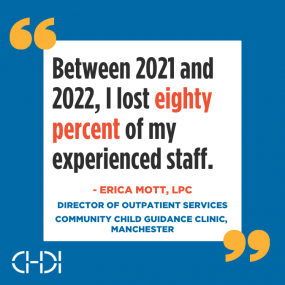
Erica Mott, LPC, Director of Outpatient Services at Manchester’s Community Child Guidance Clinic, had a similar experience. “Between 2021 and 2022, I lost eighty percent of my experienced staff,” she says. “I’m fully staffed again now, but it’s mostly with people who have graduated within the last two years.”
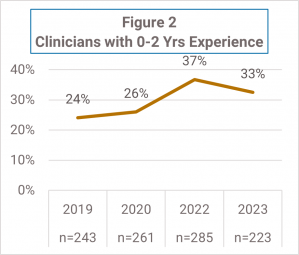
According to CHDI’s annual survey of staff from 22 OPCC providers across Connecticut, the share of OPCC clinicians with two or fewer years of experience increased from 25% in 2019 to over a third in 2022 and 2023 (see Figure 2). OPCC leaders reported more difficulty with recruitment, turnover, and the dilemma of whether to assign an influx of more challenging cases to inexperienced staff who may not have the appropriate training or add to the already full plates of their experienced clinicians.
“We went from having these seasoned clinicians who had been trained in all the evidence-based practices to starting with brand new folks,” Jacob says. “A lot of our [post-pandemic] transitions were with therapists who had never had a one-on-one, in-person session with a client. They’d only done telehealth because their entire training had been online.”
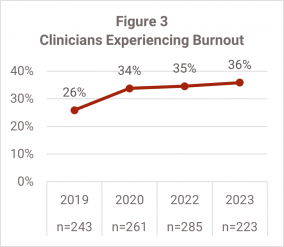
The combination of higher caseloads, increased demand and acuity, insufficient pay, and a “greener” workforce is a recipe for burnout for clinicians at all experience levels. According to our OPCC surveys, 36% of clinicians reported burnout in 2023 compared to 26% in 2019 (see Figure 3).
There are several reasons behind this shift, but stagnant insurance reimbursement rates and funding impacting OPCCs’ ability to pay competitive salaries are major factors. When combined with the state’s skyrocketing post-pandemic housing costs, the situation has also disproportionately forced younger clinicians to take on additional jobs to make ends meet, exacerbating stress and burnout.
“Some of [our younger clinicians] are coming out of grad school with $200,000 in student loans,” says Jacob. “Several of my youngest clinicians have three jobs, and they’re tired… The burnout rate is high for our younger clinicians. They can’t afford to just come in and do the job and go home. We do a lot of work on self-care. But when the system is this broken, you can self-care all you want - it’s not enough.”
For their part, many supervisors are struggling to provide the level of support for new staff that these increased demands require. Advising new clinicians who are inexperienced with risk assessment, navigating the behavioral health system, and handling more acute cases is stressful and time-consuming for supervisors, who typically also carry their own caseloads of higher acuity cases.
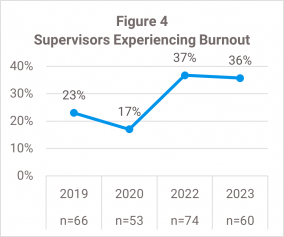
Unsurprisingly, the OPCC supervisors we surveyed are showing an even more dramatic increase in burnout, with 2023 supervisor burnout rates increasing more than 50% compared to 2019 (Figure 4). Experienced clinicians having to take on more intensive cases also means they aren’t available for new clients, contributing to the longer delays and waitlists many families across the state are facing.
“You can’t give new staff the more challenging cases,” says Mott. “You have to build that skill set… But now a lot of my more experienced staff are holding all the kids with schizophrenia, developmental trauma, [and other complex or long-term treatment cases]… it creates a backlog. The longer staff are here, the more they end up with those cases, which leaves less space for new kids to come in.”
Individual supervision plays a critical role in training and supporting newer clinicians, but many receive only an hour of supervision weekly for caseloads of 60+ children due to insufficient fee-for-service rates and a lack of reimbursement for these activities that do not support adequate supervision.
Director of Implementation Jack Lu’s recent post provides a deeper dive on how this crisis is affecting Connecticut’s most experienced clinicians and supervisors.

Connecticut must craft a new recipe that supports the entire behavioral health workforce and the families they serve. And we don’t have to create it from scratch: the Strategic Plan to Strengthen Connecticut’s Behavioral Health Workforce has all the ingredients we need. Three of the plan’s recommendations are especially relevant here:
As noted in Recommendation 5 of the Strategic Plan, research has shown that staff training can increase job satisfaction and improve retention, making it easier to retain clinicians at any experience level and supervisors. Providers surveyed for the plan indicated these areas as priorities for future training:
These professional development opportunities are particularly valuable for newer clinicians who would benefit from feeling more prepared to effectively treat populations and conditions they were not exposed to during their fieldwork. Training in one or more evidence-based practices - such as TF-CBT and MATCH-ADTC*, which are proven by rigorous research to have better, more equitable outcomes for youth compared to “usual care” – can also provide newer clinicians with clear, structured models to follow while promoting high-quality care.
For Connecticut’s OPCC network specifically, shifts in the needs of youth and families served by these providers should always inform training needs. OPCC data show that compared to pre-pandemic, the average percentage of children and youth seeking services for anxiety and trauma has grown substantially (see Figure 5). And while “disruptive behavior” problems have decreased from pre-pandemic rates, they remain the second most common primary presenting problem. 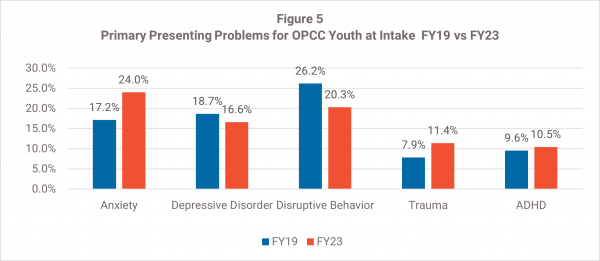
Mott says that her clinic has actually seen a post-pandemic increase in “disruptive behavior” diagnoses, but she’s not sure if that reflects increasing acuity or staff training and experience levels. “The staff pre-pandemic was very trauma-informed, but the newer staff aren’t as aware of the ways trauma [can impact behavior],” she says. At any rate, ensuring that new clinicians have training in trauma-informed, evidence-based treatments for the most common presenting problems would help meet the needs of families and clinicians alike.
Many providers have also mentioned a need for additional supervision training, which is not typically part of graduate school or field placement education. More training in supervisory skills and strategies to support staff could help supervisors be (and feel) more effective and potentially reduce burnout for them and their staff.
See Recommendation 5 in the Strategic Plan to learn more about training needs for Connecticut’s behavioral health workforce.
*TF-CBT stands for Trauma-Focused Cognitive Behavioral Therapy; MATCH stands for Modular Approach to Therapy for Children with Anxiety, Depression, Trauma, or Conduct Problems. Learn more about these EBPs here.
Connecticut should establish a centralized source of accessible training support for OPCCs and other behavioral health providers to ensure that staff training plans are informed by accurate data on the increasing behavioral health needs of youth and families, changes in demand for services, and the professional development needs of a less experienced workforce.
A statewide Children’s Behavioral Health Workforce Center – similar to the state’s Center for Nursing Workforce - would track data on the needs of families and clinicians to help develop timely, relevant training offerings that would provide the tools that this greener workforce needs to meet the needs of Connecticut families.
To learn more about the roles and responsibilities of a Behavioral Health Workforce Center and see examples from other states, see Recommendation 3 in the Strategic Plan.
Nonprofit, community-based OPCCs need higher reimbursement rates and increased state funding that will cover the true cost of providing high-quality care. Additional funding to support staff recruitment and retention would enable OPCC providers to dedicate more time to training and supervision.
Currently, overwhelmed agencies and supervisors can’t prioritize these areas as much as they’d like because they must focus on triaging higher and more severe caseloads. In the long run, this further accelerates staff burnout – and ultimately hurts the children and families who rely on OPCCs for these critical services, most of whom are already facing hardship and cannot seek services elsewhere. 70% of the youth and families served by OPCCs are enrolled in Husky, Connecticut’s Medicaid program for lower-income families.
We were pleased to see Governor Lamont’s recent announcement of a new student loan repayment program for clinical social workers and nurses and hope to see additional funds invested in the behavioral health workforce in the coming year.
Read the rest of our blog series and see Recommendation 1 in the Strategic Plan for specifics on where more investment is needed in Connecticut’s behavioral health workforce.
We have the recipe. We know the ingredients. To support our behavioral health workforce and ensure that all Connecticut youth and families can access high-quality care, now it’s time to start cooking.
This is the sixth post in our special series taking a closer look at Connecticut’s behavioral health workforce challenges and their impact on children and families – and exploring solutions. Read the rest of the series here.

|
Kellie Randall, Ph.D. - Associate Vice President, Quality Improvement krandall@chdi.org |

|
Katie Newkirk, Ph.D. - Senior Associate knewkirk@chdi.org |
CHDI offers training, technical assistance, data analysis and other quality improvement support for children's behavioral health providers and schools in Connecticut interested in offering one of the evidence-based practices mentioned in this post, including TF-CBT, MATCH-ADTC, CBITS/Bounce Back, and others. Learn more about how we support providers and contact us to get involved here.
Strengthening the Behavioral Health Workforce for Children, Youth, and Families: A Strategic Plan for Connecticut (CHDI Report, 2023)
CHDI Blog Series: Strengthening CT’s Behavioral Health Workforce (2024)
"Connecticut is Losing Our Most Experienced Community-Based Behavioral Health Providers. Here’s How We Can Keep Them." (Jack Lu, Ph.D., CHDI Blog, 2024)
Better than (Usual) Care: Evidence-Based Treatments Improve Outcomes and Reduce Disparities for Children of Color (CHDI Issue Brief, 2019)
When to Adapt: Ensuring Evidence-Based Treatments Work for Children of Diverse Cultural Backgrounds (CHDI Issue Brief, 2023)
How Trauma-Focused Evidence-Based Treatments Help Children in Connecticut (CHDI Infographic, 2022)
Directory of Evidence-Based Practice Providers for Children in Connecticut (CT DCF and CHDI)
About CHDI's Work to Expand Access to Key Evidence-Based Practices in Children's Behavioral Health